Acute Cannabinoid Intoxication (ACI) has become a widespread health issue in the United States, particularly in the increasing number of states that have legalized cannabis for medical and/or recreational use. The ingestion of large quantities of tetrahydrocannabinol (“THC”), typically via edible products is a major cause of cannabinoid intoxication and therefore a leading cause of THC-related emergency room visits.
ACI by synthetic cannabinoids (also known as “synthetics”, “K2” or “spice”). Synthetic cannabinoids are analogous to fentanyl or opioids insofar as the healthcare threat they pose to those who consume them.
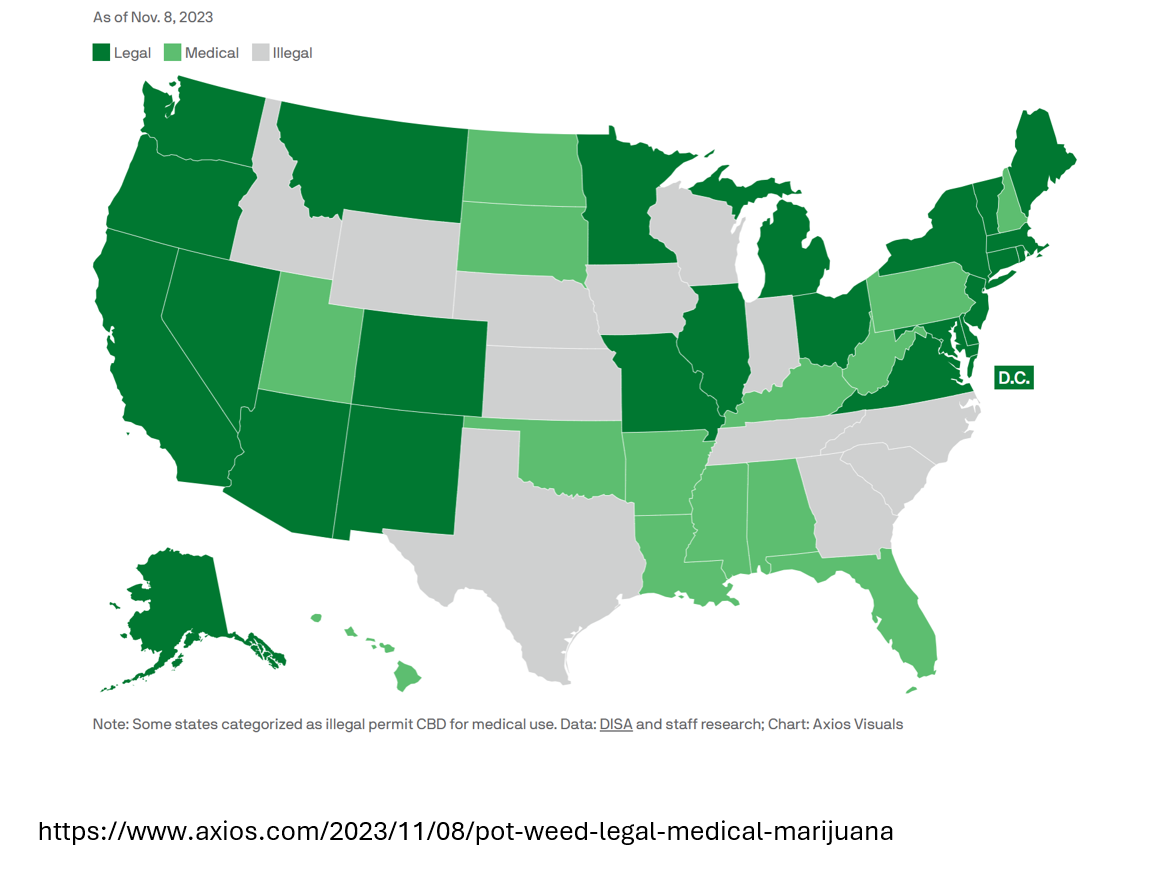
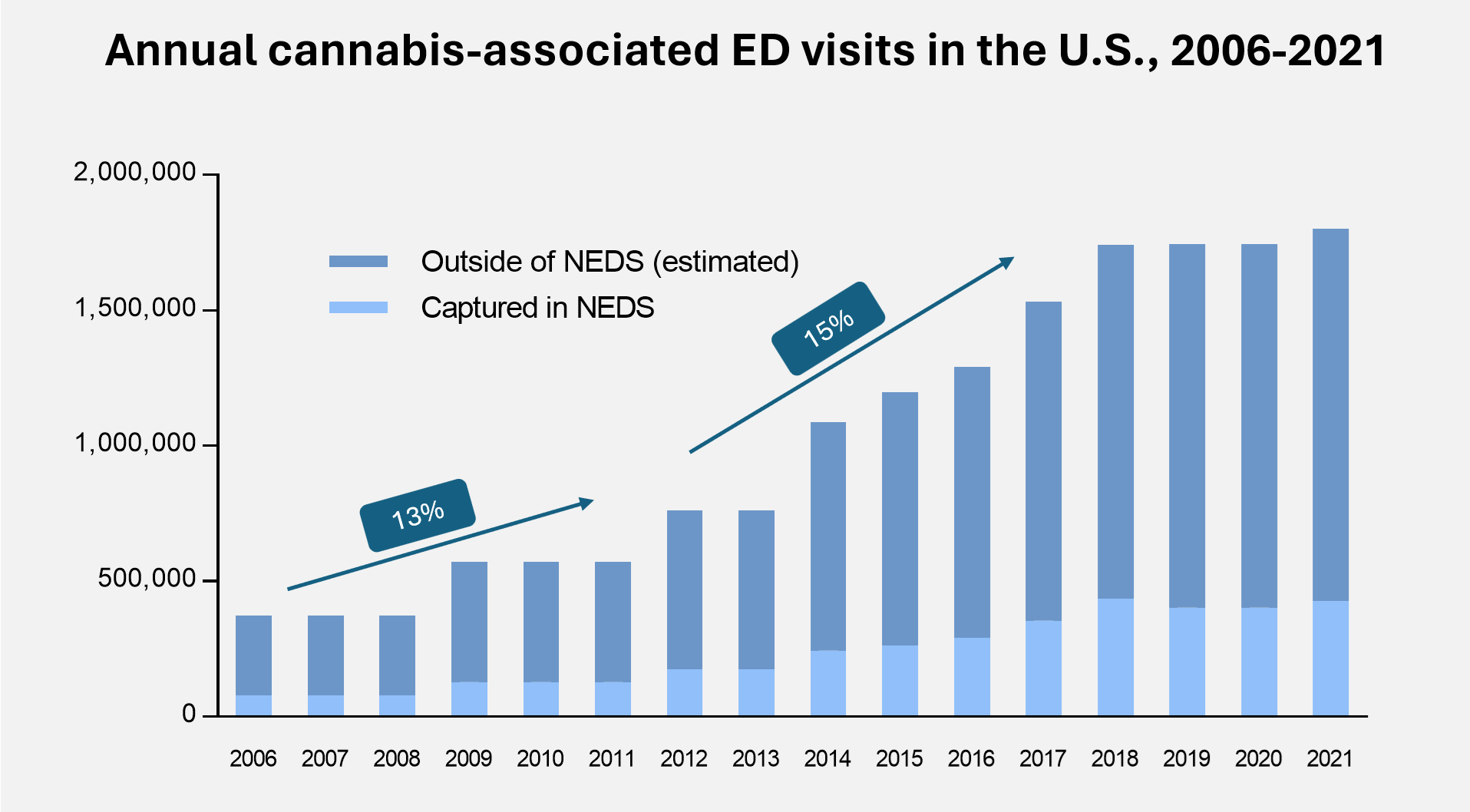
In recent years, hospital emergency rooms across the United States have seen a dramatic increase in treating patients with cannabis-related conditions. Growth of cannabis-associated emergency department (ED) visits accelerated to a 15% CAGR between 2012, when the first states legalized cannabis to 2018. After a brief plateau during COVID likely due to the avoidance of hospital exposure, however with the recent support to decriminalize we expect further growth to occur
According to a published scientific paper that provided a national estimate based on data from The Nationwide Emergency Department Sample (NEDS), the largest all-payer database in the United States that provides estimates of hospital-owned emergency department visits, the number of cannabis-associated ED visits was estimated to have surpassed 1.8 million in 2021. We believe the number of cannabis-related hospitalizations will increase substantially as more states legalize cannabis for medical and recreational use. There is an urgent need for a treatment to reverse the symptoms of acute cannabinoid intoxication and unintentional cannabis poisoning.
Prescriber research via a survey of emergency room physicians shows a significant unmet medical need for cannabinoid intoxication. According to the survey, on a scale of 0 (no need) to 10 (significant need), physicians scored on average of 7.52, indicating they believe there is a strong need for a cannabinoid antagonist to treat cannabis intoxication.
The physicians surveyed provided encouraging feedback on how useful they would find a cannabinoid antagonist in the emergency room setting:
“Have had several pediatric patients require intubation secondary to cannabis intoxication and would make a large impact on their care.”
“Can’t wait for the antidote.”
“It would help avoid intubation if respiratory depression.”
“An antagonist would be so helpful, because these patients often spend an inordinate amount of time in the ER becoming clinically sober.”
Synthetic Cannabinoids are
a Growing Problem